Pioneers of Hope
Published on September 9th, 2014 by user.
At the Monroe Carell Jr. Children’s Hospital at Vanderbilt, our physicians’ work extends beyond patient exam rooms. They are also searching for discoveries to offer better treatments, and hopefully, find cures for their pediatric patients. The doctors profiled here represent only a sampling of the physicians working tirelessly to make Children’s Hospital a place of unwavering hope. Starting this issue, we will include a profile to highlight our long-standing partnership with our community pediatricians who help ensure all children receive the best care each and every day.

For decades, the Monroe Carell Jr. Children’s Hospital at Vanderbilt has partnered with community pediatricians in Nashville and surrounding counties to ensure local children receive the very best care. One of those strong partnerships is with Old Harding Pediatric Associates and three of its long-serving practitioners—Bill Long, M.D., David Thombs, M.D., and Arville Wheeler, M.D.—now all retired.
These three men, beloved by the community and responsible for the health of thousands of children over their careers, have a long history with Vanderbilt.
Long received his undergraduate degree at Vanderbilt, went to the University of Kentucky for medical school and returned to Vanderbilt for residency.
Thombs earned his medical degree and did his residency at Vanderbilt, with one year at Cincinnati Children’s Hospital.
After medical school at Vanderbilt and residency at Cincinnati Children’s Hospital, Wheeler was the first to join Old Harding Pediatrics in 1966, then known as Overall, Strayhorn and Wheeler. The founder, James C. Overall, M.D., is a legendary figure in Nashville pediatrics, and in fact, has an endowed chair position at Vanderbilt named after him. Steven Webber, MBChB, MRCP, chief of Pediatrics at Vanderbilt, is the James C. Overall Professor.
“Dr. Overall and my father-in-law were golfers together,” Wheeler recalled. “After my training, I just went to say hello and had sat in his chair for 2 minutes when he asked me to go into practice with him. That changed everything.” Wheeler credits Overall with developing the close relationship between the hospital and the community pediatricians that continues today.
“Dr. Overall stressed the ‘town and gown’ relationship, everyone working together. There was always a wonderful relationship,” Wheeler said.
Wheeler invited Thombs, who he knew from residency in Cincinnati, to join the practice in 1969 as it was clearly outgrowing its location on Church Street. A developer offered land on Old Harding Road, where the group thought children would enjoy watching the trains roll by on nearby tracks. Old Harding Pediatric Associates was born in 1974.
The practice continued to grow rapidly, adding a new pediatrician every three or four years, including a very impressive former intern named Bill Long.
“He had a very sick baby (a patient) with Group B streptococcal septicemia. It was not well-known at the time, but Bill, who was just an intern, knew more than anybody else in the hospital and we knew we had to recruit him,” Thombs recalled.
Long took seriously the partnership between Vanderbilt and community pediatricians, including attending Grand Rounds as chief resident, writing a summary and distributing it to the local pediatricians’ offices. The reason for going above and beyond was simple for him: “I just love kids and want to be sure they get the best care.”
Old Harding pediatricians welcomed Vanderbilt medical students and residents into its practice to observe and learn, and also took time to teach at Children’s Hospital.
“Our connection was not just as community pediatricians but also as teachers. The ‘clinical faculty’ attached to our title had meaning, and we took seriously the invitation to be co-attending physicians on rounds once a month. We were paired with faculty and could give viewpoints from a specialist and a practicing pediatrician,” Thombs said.
Wheeler recalled that when he was an intern, there were 12 pediatricians on the Vanderbilt faculty. Now there are hundreds in many different specialty fields. Despite the growth and change, the strong partnership and communication remains.
“The Vanderbilt faculty is so great to call us back and communicate, and let us be a partner with them. The departments grew quickly and many of the new doctors didn’t know who we were but still communicated and kept that personal relationship,” Thombs said.
Since their retirement, the Old Harding legacy continues with three office locations and 10 pediatricians, including Long’s son, John Long, M.D.
“This town is blessed with gobs of great pediatricians,” Bill Long said. “We’re just one group of many, and we are all more friends than competitors and felt the same way about the Children’s Hospital.”
– by Leslie Hill
•••

While the immediacy and intensity of caring for newborns in the Neonatal Intensive Care Unit at Monroe Carell Jr. Children’s Hospital at Vanderbilt appeals to Stephen Patrick, M.D., MPH, he is equally interested in understanding how and why the tiny infants ended up there in the first place.
Of particular concern to him are the babies who suffer complications from drug withdrawal due to their mothers’ opiate dependency.
“What I see in our health system repeatedly is we react to health problems after they have occurred. My hope is that in drawing attention to drug withdrawal, rather than putting the shame and blame on the mom, we think about this as a problem that should be addressed way before infants arrive in the NICU,” said Patrick, who came to Vanderbilt in July 2013 from the University of Michigan.
Patrick attended the University of Florida, where he started out as an engineering major. He liked to tinker with things and figure out why they worked—and why they didn’t. This natural curiosity served him well as he changed course, attended medical school and took a year off to earn a Master of Public Health degree from Harvard.
“In medical school, it was evident that there was an entire health system around my patients that was affecting them. I took off a year to get a better understanding of how our health system works, how things interact, and hopefully, how to make things better.”
Patrick, assistant professor of Pediatrics, completed a pediatrics residency at the University of Michigan and a fellowship in neonatology. He participated in the Robert Wood Johnson Clinical Scholars program for physicians interested in health services and health policy research.
“You can see in our NICU the problems that we take care of are just a microcosm of what is happening around us when you think about prematurity. It’s more a story of poverty and bigger, broader questions that need to be addressed to improve outcomes for our infants.”
As a neonatology fellow he began to observe more infants having drug withdrawal from prescription opioids. He studied national trends and found that the diagnosis rate tripled over the last decade, reaching one infant per hour in the United States by 2009, accounting for $720 million in health care expenditures.
“That’s where that translational piece happens that’s so important for me: to take something that we see at the bedside and put some data to it to influence policymakers,” said Patrick, who spends 75 percent of his time conducting research.
He recently received a Department of Health grant to build a predictive model for infants developing drug withdrawal based upon maternal prescribing factors. About 30 percent of mothers enrolled in Tennessee’s Medicaid program have at least one legal prescription for opioids.
“That’s part of my interest—engaging with folks in Tennessee to figure out how we begin to control this problem and begin to think about it from a public health perspective.”
Outside the NICU, Patrick enjoys spending time with his family, including two daughters, ages 8 and 3. He enjoys woodworking and kayaking and discovering what Nashville has to offer, including the hiking trails at Percy Warner Park.
“Nashville is a perfect match for us. We love it. I am so grateful for the amazing amount of support I’ve received from Vanderbilt,” said Patrick, who recently spent a month in the White House Office of National Drug Control Policy. “This is a testament of how supportive Vanderbilt is of junior faculty and this issue.”
– by Kathy Whitney
•••

On July 1, a fresh crop of pediatric residents arrived on the Vanderbilt University Medical Center campus for their first day of work. They were greeted by Rebecca Swan, M.D., who will mentor, monitor and even, to some extent, mother them for the next three years.
Swan is the pediatric residency program coordinator, a position she has held since 2002. She oversees 72 residents and is responsible for their training. Watching these young physicians grow in competency and confidence is her favorite part of the job.
“The residents come in and learn skills, but even better, they learn to feel confident with those skills,” Swan said. “The faculty members take pride in them. They are like our children.”
Swan completed medical school at the Medical College of Virginia and went on to residency training, followed by a year as chief resident at Keesler Air Force Base in Mississippi. She spent three years in a community military practice in Phoenix before moving to Nashville in 1997 to pursue a career in academic pediatrics. She became Associate Residency Program Director in 2000 and took over the helm in 2002.
Her workday varies weekly and even seasonally. Every day begins with a 7:45 a.m. teaching conference with all of the pediatric residents. November through January is busy recruitment season during which Swan interviews more than 200 fourth-year medical students vying for 23 internship spots.
She spends a lot of time designing the residency program curriculum and plays a significant role in faculty development across the Graduate Medical Education continuum. Interspersed with her administrative duties are the day-to-day responsibilities of helping residents who have personal issues, a challenging case, a bad patient outcome or patient affairs concerns.
“There is a lot of unpredictability to what I do, but I like that,” she said.
The one constant in her week is seeing patients in clinic every Tuesday morning. “I think it’s important that I still see patients, and I love doing that. I would not want to lose that.”
Swan and her husband, Michael Swan, M.D., have two children, a son and a daughter, both 12. The couple’s firstborn, Johanna, died at age 14 months, and the family was inspired to establish a memorial to her while simultaneously helping economically disadvantaged families.
Jo’s Reach Out and Read Book Club was founded in memory of Johanna in February 2000 at what was then known as Vanderbilt Children’s Hospital, currently Monroe Carell Jr. Children’s Hospital at Vanderbilt. It provides age-appropriate books free to children at well-child visits, encourages parents to read to their children and offer guidance, and models good reading behavior by providing volunteers to read to children in clinic waiting rooms.
Swan is a literacy proponent and loves to read in her free time. She and her family travel extensively and plan to travel to Alaska this summer.
Among her many interests and varied responsibilities, interacting with the residents brings her the most satisfaction.
“The residents are why I get up and come to work in the morning. They are bright, ambitious, and they really want to do the best for the kids they care for,” she said.
– by Kathy Whitney
•••

David Morrison’s passion for medicine traces back to a high school career exploration program when a neuroendocrinology investigator exposed him to surgical research.
He knew instantly he wanted to be a doctor. Today he cares for children’s vision as a pediatric ophthalmologist at the Tennessee Lions Eye Center at the Vanderbilt Eye Institute.
Morrison, M.D., associate professor of Ophthalmology and Pediatrics, came to Vanderbilt in 2003 as the first pediatric ophthalmology fellow. He now directs the fellowship program and maintains a robust research portfolio while caring for his young patients.
“People take sight for granted, and don’t really understand how important it is until it is gone. The benefit of doing pediatrics is that you provide that child with a lifetime of vision,” Morrison said.
“I have the opportunity to treat many children born with cataracts (cloudiness in the lens of the eye) who can see no more than light. I get to do a surgery and take a patch off their eye the next day and watch them open their eyes and see their mom’s face for the first time. That’s cool.”
As a leading center in delicate pediatric cataract surgery, Morrison performs the majority of pediatric cataract surgery in the region. He is also an expert in retinopathy of prematurity (ROP), the abnormal growth of blood vessels in the eyes of preterm infants, which can lead to blindness. It can be treated with laser surgery or the injection of a medicine that counteracts a chemical called vascular endothelial growth factor (VEGF).
“Anti-VEGF medicines decrease the chemical signal for new blood vessel formation, but the injection is not only stopping the abnormal blood vessels from growing, but the normal blood vessels too,” he said. “I’ve done basic science research looking at different forms of VEGF and how those different forms may affect the development of ROP. That’s something that may guide us in developing new technologies and new drugs to treat ROP while sparing the normal blood vessels.”
An important factor in ROP treatments is early detection screening. Morrison is involved with two studies looking at screening methods. The first tests the feasibility of using a special camera to photograph the eye and then evaluating the photo at a central location.
“Using the camera and a central reading site could represent a real paradigm shift in ROP care. Current screening models require many infants to be transported to Vanderbilt from outside NICUs. If we could provide the service remotely, we could allow these children to stay closer to home and closer to their families.”
The second study examines the relationship between an infant’s growth rate and their risk of developing severe ROP.
“We’ve noticed that you can monitor how the baby grows shortly after birth as a surrogate of growth factor deficiency. These same growth factors are associated with the development of ROP. If the baby is not growing the way they should be, we can predict who is at highest risk for developing severe ROP.”
Morrison graduated from University of Kentucky College of Medicine and did his residency training at University of Alabama at Birmingham.
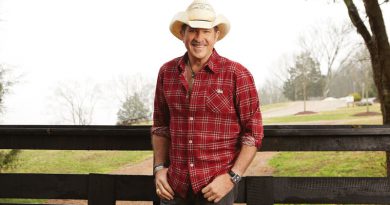
After spending his days operating on eyes, Morrison leaves the hospital to “operate” on old houses. He lives with his wife and two daughters in homes while he remodels them. His current project is about seven years in the making.
“I bought a house in Franklin that was built by a country singer in the 70s, good bones on good land but a lot of black and gold fleck tile, wood paneling and really ugly stuff. I go one room at a time and strip it down to the studs and start over,” he said.
“It’s very similar philosophy to surgery. You’re working with your hands to make something better.”
– by Leslie Hill